Quick promise: If you’ve ever lain awake at 3 a.m. while your partner snores like a chainsaw—or bolted upright after a nightmare—this guide explains why sleep goes sideways and, more importantly, how to set it right.
CTA: Download our free printable Sleep Symptom Tracker to start spotting patterns tonight.
What Is a Sleep Disorder?
Definition & Diagnostic Criteria
A sleep disorder is any persistent change in the way you fall asleep, stay asleep, or feel during the day that meets thresholds in the International Classification of Sleep Disorders (ICSD‑3) and the DSM‑5. The American Academy of Sleep Medicine guidelines break down the technical checklist in plain English.
Prevalence & Impact on Health
Roughly 1 in 5 adults worldwide wrestle with a diagnosable sleep issue. Poor sleep doubles long‑term risk for heart disease, depression, and type 2 diabetes (Frontiers in Psychiatry, 2025). The Centers for Disease Control and Prevention sleep statistics slice the numbers by age and gender.
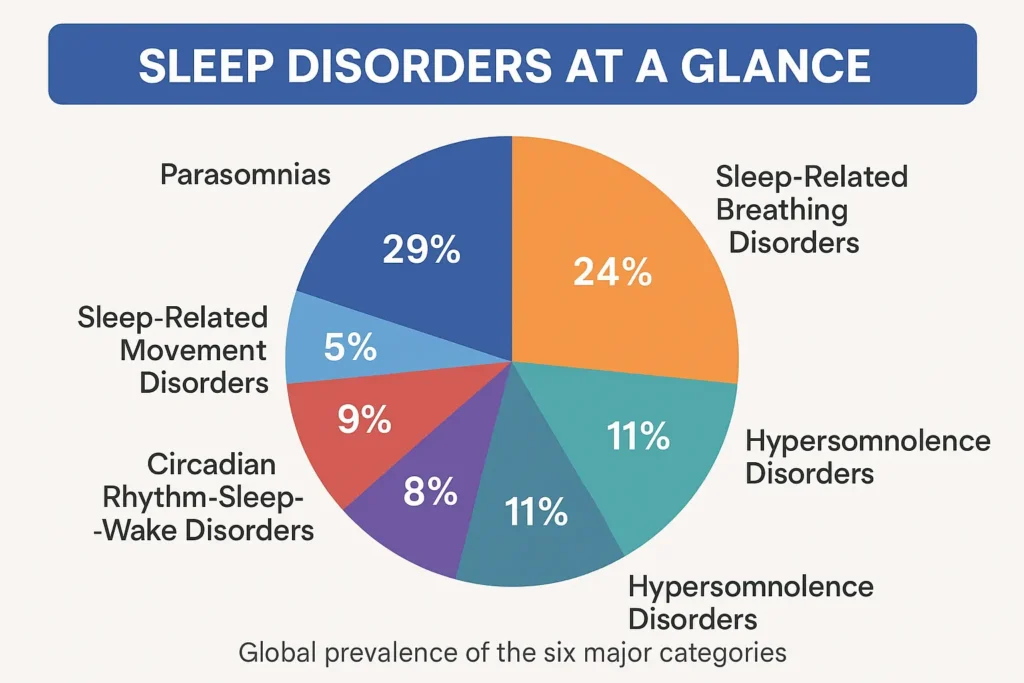
Approximate Pie Chart of Worldwide Sleep Disorders
Classification of Sleep Disorders
| Category | Key Night‑time Sign | Daytime Fallout |
|---|---|---|
| Insomnia Disorders | Trouble falling/staying asleep ≥3 nights/week | Fatigue, brain fog |
| Sleep‑Related Breathing Disorders | Loud snoring, breathing pauses | Morning headaches |
| Hypersomnolence Disorders | Sudden sleep attacks | Automatic behaviour |
| Circadian Rhythm Disorders | Sleep‑wake clock out of sync | Jet‑lag feeling daily |
| Parasomnias | Undesired events (walking, acting out dreams) | Safety hazards |
| Movement Disorders | Irresistible limb urges | Fragmented sleep |
[⚡ MYTH‑BUSTER:] “Snoring is harmless.” Persistent, loud snoring often flags obstructive sleep apnea (OSA)—a condition that strains heart and brain alike. Snoring is NOT cute or amusing, if you’re snoring regularly, at the very least track your sleep so you can ascertain how it may be impacting your sleep cycles.
Insomnia
Types (Acute vs. Chronic)
Acute bouts last days to weeks—often after stress or travel. Chronic insomnia sticks around ≥3 months and needs structured care.
Symptoms & Daytime Effects
Clock‑watching, frequent early wakings, mood swings, microsleeps.
Common Causes & Risk Factors
Stress, late caffeine, blue‑light exposure, pain, pregnancy, menopause. Circadian rhythm misalignment is another huge reason due to shift work, jet lag, late night socialising often made worse with alcohol (aka “social jet lag”) or just generally staying up too late.
Diagnosis & Assessment
Keep a two‑week sleep diary or complete the online Insomnia Severity Index questionnaire before seeing a clinician.
Treatment & Management
Cognitive Behavioural Therapy for Insomnia (CBT‑I)
The gold standard—stimulus control, sleep‑restriction windows, paradoxical intention.
Medications & Supplements
Short‑term use only: doxepin, dual orexin‑receptor antagonists, low‑dose melatonin.
Sleep Hygiene Strategies
- Dim lights 90 min before bed
- Caffeine curfew 2 p.m.
- Consistent wake‑time—even weekends
- Morning sunlight upon waking
[📋 Nightly Reset Checklist] Five‑step wind‑down you can paste to your nightstand.
Prevention & Self‑Help Tips
One of the more overlooked reasons for insomnia is circadian rhythm misalignment. When you fall asleep..and when you wake up…is for the most part directed by your endocrine system and the two important hormones it produces..namely melatonin in the evening to send you to sleep, and cortisol in the morning to wake you up.
With modern living, it’s so easy for our circadian rhythm to get “out of whack”…
I should know – because for so long, this was the one thing that messed up my sleep so much.
During covid I would barely leave the house, my body didnt know when it was daylight or nighttime, so it would produce cortisol in the evening and melatonin in the morning.
Mornings took me an age to get moving because my peak cortisol production had been hours before…and my peak melatonin production was in the early morning.
Not to mention I was staying up too late regularly.
When I got up and when I went to sleep was all over the place.
Its easy to reset though – go to bed at the same time. Get up at the same time (as much as you can..)…
….and get sunlight in your eyeballs as early as you can in the day (to kick start that melatonin production…which in turn starts the cortisol production process..)
Sleep‑Related Breathing Disorders
Obstructive Sleep Apnea (OSA)
Repeated throat collapse → oxygen dips, micro‑arousals, epic “wake the dead” snoring.
Central Sleep Apnea & Snoring
Brain occasionally forgets to breathe—common in heart‑failure patients.
Symptoms & Health Consequences
Partner‑reported pauses, gasping awakenings, hypertension, stroke risk.
Diagnosis (Polysomnography or Home Testing)
One night in a sleep lab—or an FDA‑cleared home kit—measures the apnea–hypopnea index (AHI). Pulse oximeter will also give an indication of blood oxygen drops during sleep ( however this NOT count as a proper medical diagnosis….more of an indication). Same goes for sleep trackers like Whoop, Fit Bit, Oura Ring etc
Treatment Options
CPAP & BiPAP Therapy
Gentle air pressure keeps the airway open.

Oral Appliances & Lifestyle Changes
Mandibular advancement devices, weight loss, side‑sleeping, breathing “re-training”
[⚡ MYTH‑BUSTER:] “CPAP machines are noisy and impossible to wear.” Modern units whisper at <26 dB—quieter than a fridge—and masks now come in minimalist under‑nose designs.
Hypersomnolence Disorders (Excessive Sleepiness)
Narcolepsy
Autoimmune loss of hypocretin cells; classic cataplexy in Type 1.
Idiopathic Hypersomnia & Kleine–Levin Syndrome
Extreme sleepiness without REM intrusions; KLS causes cyclical “sleep marathons.”
Symptoms & Triggers
Sleep attacks, automatic behaviour, brain‑fog “banks” after naps.
Diagnostic Work‑up
Multiple Sleep Latency Test, HLA typing for narcolepsy.
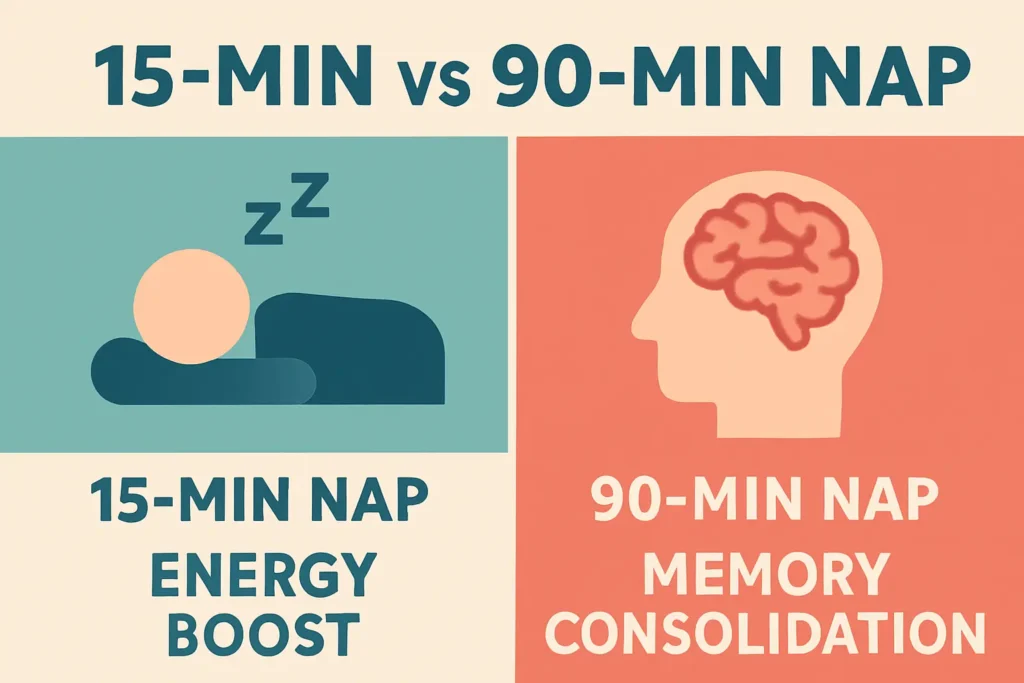
Management Strategies (Stimulants, Scheduled Naps)
Modafinil, low‑sugar diet, 20‑min “power‑anchors.”…and lots of coffee.
Circadian Rhythm Sleep–Wake Disorders
Shift‑Work Disorder
Night shifts desynchronise the body clock—accident risk rises 37 %.
Jet Lag
Rule of thumb: one time zone per day for recovery—eastward flights hurt more.
Delayed & Advanced Sleep Phase Disorders
“Night‑owl” vs “early‑bird” biology taken to the extreme.
Non‑24‑Hour Sleep–Wake Rhythm
Mostly in totally blind individuals—body clock >24 h.
Symptoms & Functional Impact
Social jet‑lag, performance dips, irritability.
Treatment & Coping Techniques
Light Therapy & Melatonin Timing
10 000 lux box on wake‑up; 0.5 mg melatonin 5 h before target bedtime. Ultimately though – the best remedy is to reset one’s circadian rhythm as soon as possible by waking up in and around dawn and going to bed a few hours after sunset.
Behavioural Scheduling
Strategic naps, anchored mealtimes.
Parasomnias
REM Behaviour Disorder (RBD)
Acting out vivid dreams—may foreshadow Parkinson’s.
Sleepwalking, Sleep Terrors & Confusional Arousals
Complex behaviours with no memory the next morning.
Nightmares & Sleep Paralysis
Intense fear or temporary inability to move on waking.
Causes & Safety Considerations
Genetics, medications, stress, alcohol, unsafe bedroom setup.
Management & When to Seek Help
Scheduled awakenings, safety locks, clonazepam for severe RBD.
[📋 Safe Bedroom Setup] Remove trip hazards, install motion‑sensor night‑lights.
Sleep‑Related Movement Disorders
Restless Legs Syndrome (RLS)
Creeping limb sensations, relieved by movement—often worse at rest.
Periodic Limb Movement Disorder (PLMD)
Involuntary leg kicks every 20–40 seconds during NREM sleep.
Bruxism & Sleep Leg Cramps
Teeth grinding or sudden calf spasms that jolt you awake (often related to stress or sleep apnea..)
Symptoms, Triggers & Quality‑of‑Life Impact
Iron deficiency, pregnancy, SSRI use; can rack up 20 000 muscular twitches in a single night.
Treatment Options (Iron Supplementation, Medications)
Ferritin > 75 ng/mL target; dopamine agonists, alpha‑2‑delta ligands.
[⚡ MYTH‑BUSTER:] “Only older adults get RLS.” It often peaks in mid‑life women and can start in childhood.
Diagnosis of Sleep Disorders
Clinical Sleep Studies (Polysomnography, Actigraphy)
Gold‑standard overnight monitoring vs multi‑day wrist‑worn motion sensors.
Screening Questionnaires & Diaries
Epworth Sleepiness Scale, STOP‑BANG, app‑based logs.
Specialty Referral & Sleep Clinics
When self‑help stalls, ask for a board‑certified sleep physician or use the AASM “Find a Facility” tool.

Living with a Sleep Disorder
Lifestyle Adjustments & Sleep Hygiene
Regular exercise, evening wind‑down rituals, alcohol moderation.
Self‑Help Strategies & Support Groups
Peer forums like Narcolepsy Network and MyApnea.org ({{LINK_NEEDED}}).
When to Consult a Professional
Breathing pauses, violent parasomnias, or insomnia lasting >3 months.
Frequently Asked Questions
Can sleep disorders be prevented?
Not all—but solid sleep hygiene slashes risk for acute insomnia and jet‑lag.
What causes sleep paralysis?
A brief glitch where REM muscle atonia out‑lasts waking
Is snoring a sign of disease?
Habitual, loud snoring may indicate OSA—get screened.
How do I choose the right specialist?
Look for AASM accreditation or a neurologist with a sleep-medicine subspecialty.