Why Sleep Matters for Mental Health
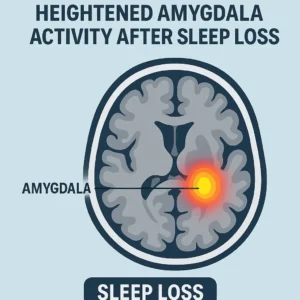
Emotional Regulation & Stress Response
When we skimp on shut‑eye, our brain’s chief “calm‑down” centre—the pre‑frontal cortex—loses its grip on the amygdala. The result? Sharper mood swings and a hair‑trigger stress reaction after even one night of total sleep loss (36‑hour sleep‑deprivation study). Think of it as letting the toddler drive the car while the adult naps in the back seat.
Cognitive Function & Brain Fog
Memory, focus, and decision‑making consolidate during deep non‑REM and dream‑rich REM cycles. Miss them and you’ll feel the familiar cotton‑wool brain the next day. If that sounds a lot like our Sleep Fundamentals crash course, that’s because it is—catch the recap here..
Mood Stability & Psychotic‑Like Symptoms
Chronic restriction (think 5–6 hours a night for a week) can spark micro‑hallucinations, paranoia, and dissociation—symptoms that disappear once healthy sleep returns. Your mind isn’t “broken”; it’s simply starved of REM.
I personally know what this is like – I suffered from Upper Airway Resistance Syndrome for years, I would wake up after 5, 5 and a half hours, right in the middle of REM sleep. Physically I felt “rested” – but mentally, anything but. I couldnt focus, my mind was effectively mush, words would be hard to prise out of my mind, my mind was blank.
How Mental‑Health Conditions Disrupt Sleep
Depression & Insomnia
Over 75 % of people with major depressive disorder wrestle with insomnia or early‑morning waking. Night‑owl chronotypes are at even greater risk (meta‑analysis, Journal of Affective Disorders, 2025). The cycle is vicious: sadness shortens sleep, and short sleep deepens sadness.
Anxiety & Hyper‑Arousal
Anxious brains pump out cortisol long after lights‑out. Elevated bedtime cortisol predicts up‑to‑30 % longer sleep‑onset latency (EndoText review). A calming pre‑sleep ritual (see Practical Tips) helps coax those stress hormones back into their cages.
PTSD, Nightmares & Trauma‑Related Awakenings
Trauma survivors often relive distressing memories in REM, jolting awake before the dream resolves.
Veteran describing “combat dreams”
Brad, 41, served with the U.S. Army during the invasion of Iraq in 2003. Even now, two decades later, the desert is never far from his mind. Sleep is the hardest part.
Most nights, Brad falls asleep only to be yanked awake by the same dream—convoys on dusty roads, the sudden crack of gunfire, the adrenaline rush that once kept him alive. In the dream he’s back there, hyper-alert, scanning rooftops, waiting for the next explosion. His heart pounds so hard it wakes him before the dream ends.
By morning, he’s exhausted, though he technically “slept.” His wife says he thrashes in bed, sometimes shouting. Brad hates the guilt that creeps in when his nightmares wake her, too. He’s tried earplugs, late-night TV, even pacing the backyard in the cool dark until dawn breaks. Nothing stops the combat dreams.
Brad says the war taught him to survive without much sleep—but living in peacetime with fractured nights feels like another battle altogether. Some mornings he looks at his kids eating cereal at the kitchen table and feels both grateful and hollow. Sleep, for him, isn’t rest. It’s a minefield.
Imagery rehearsal therapy (IRT) reshapes nightmare scripts and cuts nightmare frequency by ~60 %; we’ll link a how‑to guide.
Bipolar Disorder & Sleep‑Wake Phase Shifts
In bipolar I & II, manic bursts often start with a dramatic cut in total sleep time. Bright‑light exposure at structured times plus melatonin agonists (e.g., agomelatine) can stabilise circadian drift (systematic review, Psychiatry Research, 2025).
ADHD, Impulsivity & Sleep Initiation
Restless minds make restless nights. Up to 70 % of adults with ADHD report trouble “switching off.” Behavioural wind‑down routines and low‑dose evening exercise reduce sleep‑onset latency by ~15 minutes (randomised trial, Sleep Medicine, 2024).
Eating Disorders & Nocturnal Disruption
Malnutrition and electrolyte imbalance can trigger night‑time muscle cramps and awakenings. Care should focus on restoring balanced nutrition alongside cognitive therapy.
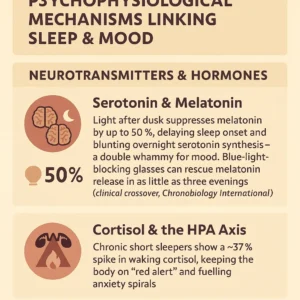
Psychophysiological Mechanisms Linking Sleep & Mood
Neurotransmitters & Hormones
Serotonin & Melatonin
Light after dusk suppresses melatonin by up to 50 %, delaying sleep onset and blunting overnight serotonin synthesis—a double whammy for mood. Blue‑light‑blocking glasses can rescue melatonin release in as little as three evenings (clinical crossover, Chronobiology International, 2024).
Cortisol & the HPA Axis
Chronic short sleepers show a ~37 % spike in waking cortisol, keeping the body on “red alert” and fuelling anxiety spirals.
Brain‑Network Changes (Default‑Mode, Emotional Circuits)
Default‑mode network (DMN) hyper‑connectivity during sleep loss mirrors patterns seen in rumination‑heavy depression. Normalising sleep helps re‑balance DMN‑task‑positive switching.
Inflammation, Gut‑Brain Axis & Sleep
Just five nights of 4‑hour sleep increased bloodstream lipopolysaccharide levels and pro‑inflammatory IL‑6 in a 2025 crossover study, pointing to gut‑leakiness as a mood risk factor (Gut Microbes, 2025).
Individual Differences & Emerging Trends
Chronotypes: “Larks” vs. “Owls” & Personalised Needs
Night‑owls operating on lark schedules face constant social jet‑lag. Aligning work hours with chronotype improved mood scores by 19 % in an Australian cohort study.
Coronasomnia: Pandemic‑Related Sleep Disturbances
Insomnia rates peaked above 30 % during COVID‑19 and haven’t fully returned to baseline, especially among women (global meta‑analysis, 2024).
Cultural Attitudes: Sleep Deprivation as a Productivity Badge
“I’ll sleep when I’m dead” may win hustle points, but chronic 6‑hour nights cost the US economy an estimated $411 billion annually in lost productivity (RAND Corporation).
Evidence‑Based Treatments & Strategies
Cognitive Behavioural Therapy for Insomnia (CBT‑I)
Online CBT‑I modules cut Insomnia Severity Index scores by 7 points in veterans, rivalling in‑person care (VA randomised trial).
Mindfulness, Meditation & Relaxation Techniques
A daily 10‑minute body‑scan lowered bedtime heart rate by 8 bpm in beginners—see our guided audio.
Pharmacological Options & Natural Supplements
- Short‑term hypnotics (z‑drugs) offer relief but risk dependency.
- Melatonin & Agomelatine help re‑sync circadian timing.
- Magnesium L‑threonate shows promise for anxiety‑related insomnia, but evidence is early‑stage (pilot study, Nutrients, 2024).
Nutritional Approaches: Foods to Encourage or Avoid
Tart‑cherry juice, kiwi fruit, and high‑glycaemic rice meals 4 hours pre‑bedtime each shortened sleep‑onset latency by 15–25 minutes across small RCTs.
Light Therapy, Chronotherapy & Scheduling
Timed 10 k‑lux exposure at 07:00 re‑shifted delayed‑sleep‑phase by 1.4 hours within two weeks; combine with nightly melatonin for best effect.
Integrating Sleep Hygiene for Mental Well‑Being
For a room‑by‑room checklist, hop over to our Sleep Hygiene pillar
Practical Tips for Improving Both Sleep & Mental Health
Establishing a Calming Bedtime Routine
- Dim lights 90 minutes before bed.
- Swap doom‑scrolling for low‑stakes fiction reading.
Screen‑Time & Stimulus Control
Evening device use over 2 hours correlated with a 13 % rise in depressive symptoms among teens (longitudinal study, JAMA Pediatrics, 2024). Blue‑light filters plus phone‑free wind‑down time are low‑hanging fruit.
Stress‑Reduction Practices (Breathing, Journaling)
The 4‑7‑8 breath slows heart‑rate variability into a parasympathetic range; pair with 5‑minute gratitude journaling for an optimism boost.
Tracking Progress: Diaries, Apps & Wearables
Devices like Oura Ring, Whoop and Apple Watch now flag heart‑rate‑variability dips that can precede mood slumps by 24 hours—valuable early‑warning data.
Frequently Asked Questions
- Can improving sleep alone alleviate depression or anxiety?
Quality sleep boosts therapy outcomes and medication response—but rarely replaces them. View it as a force‑multiplier. - Are certain foods proven to boost sleep quality?
Kiwi, tart‑cherry, and glycaemic‑indexed starches show modest latency benefits; caffeine fade‑out by 14:00 is still rule #1. - How much sleep do individuals really need?
7–9 hours for most adults, though genetics and chronotype shift the sweet spot. - What if I “bounce back” better on less sleep?
Short sleepers (<6 h) who feel fine still show higher blood pressure, insulin resistance, and mood volatility long‑term.
Further Resources & Related Guides
- Deep Dive: CBT‑I step‑by‑step workbook
- Chronotypes Explained: Are you a lark, owl, or hummingbird?
- Supplement Guide: Melatonin, magnesium, and beyond
- Condition‑Specific: Managing sleep with PTSD, ADHD, bipolar